John Gibbons, BSc (OST) – The ‘Bodymaster’
Shoulder impingement – or subacromial impingement as it is sometimes referred to – is caused by a compression of structures located within the subacromial space (rotator cuff, long head of biceps and subacromial bursa) and the coracoacromial ligament. And it’s all too common; general consensus is that 50–60% of patients presenting with shoulder complaints are suffering from an impingement of some sort. If you are a physical therapist, you likely see it every day: the cricketer who is struggling to bowl, the lady who cannot do up her bra, the person who says their shoulder pain constantly wakes them at night. But without access to MR imaging, how do you diagnose it? And more importantly, how do you treat?
What is shoulder impingement?
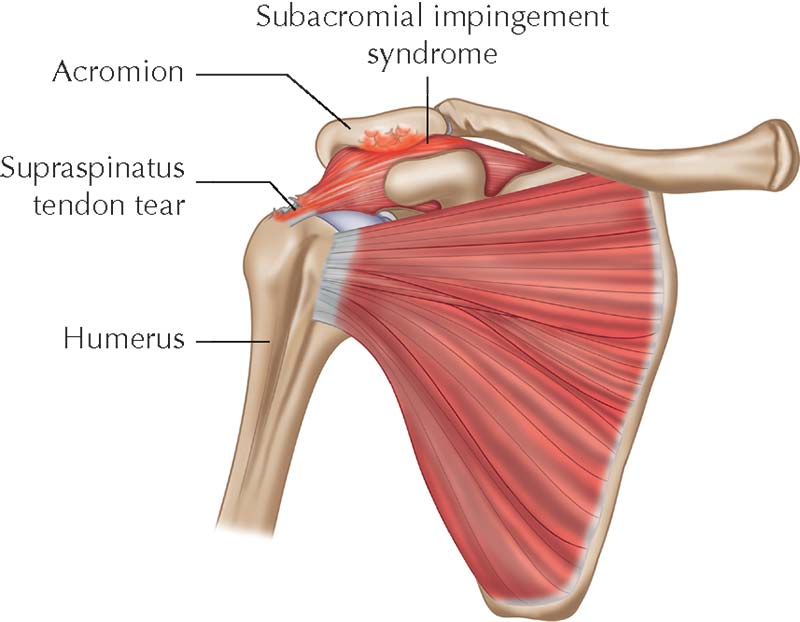
Shoulder impingement is a broad term, but generally falls in to two categories: structural and functional. A structural impingement is caused by a narrowing of the subacromial space due to bony growth or soft tissue inflammation, whereas a functional impingement is the result of muscle weakness and/or imbalance. Most commonly, the supraspinatus gets caught underneath the acromion – what you will hear patients describe as a ‘catching’ when they abduct their arm. Dr Janda illustrates the pattern of muscle imbalance neatly with his ‘upper crossed syndrome’: he describes a weakness of the lower and middle trapezius, serratus anterior, infraspinatus and deltoid muscles and tightness of the upper trapezius, pectorals and levator scapulae. It is a fascinating area however, in practice, dealing with a shoulder impingement is not always easy and usually not a ‘quick fix’.

Assess, don’t guess!
A thorough assessment of your patient is essential to gain as clear an understanding of their individual musculoskeletal biomechanical framework as possible. The examination protocol I personally follow in my clinic at the University of Oxford is detailed in my book, ‘The Vital Shoulder Complex – An Illustrated Guide to Assessment, Treatment and Rehabilitation’, and includes all active range of motion, passive range of motion, resisted tests for the glenohumeral joint and shoulder girdle, and special orthopaedic tests that I prefer to use. Resisted testing, for example, tests the integrity of the different muscular and tendinous components. Assessing joint end feel can reveal more about possible pathologies within the joint and may indicate that further investigation is needed. Drilling down with tests like the Jobe’s Empty Can test, Speed’s and Yergason’s tests will enable you to assess damage to the supraspinatus tendon, consider a SLAP lesion, and involvement of the bicipital tendon. Your assessment should reveal all the information that is relevant; take your time with it.

Treatment protocols
You may be able to help your patient in just one session, but more likely it will take time to gather all pieces of the puzzle, test your ‘hypotheses’ and evaluate the results. Patience is key. There are a lot more treatment protocols available to the physical therapist than the surgeon and my advice is to initially take one or two tools out of your toolbox, and see whether they reduce the symptoms. If that does not work, you can take out another tool, and another, until you find what does. Only after you have exhausted all the tools would you consider referring to a surgeon. In ‘The Vital Shoulder Complex’ I explain in detail the protocols which in my experience are most beneficial: METs and soft tissue techniques to address imbalances in the rotator cuff, how to align/re-position the humerus, kinesiology taping and of course rehabilitation exercises to mobilise and strengthen the shoulder girdle. Make sure you communicate clearly with your patient so that they understand what you are doing, why you are doing it and commit to keeping up their side of the partnership with any rehab exercises. That you cannot do for them!
More in-depth information on how to assess, diagnose and treat shoulder impingement and other pathologies of the shoulder and cervical spine can be found in John Gibbons’ book, ‘The Vital Shoulder Complex – An Illustrated Guide to Assessment, Treatment and Rehabilitation’.





0 Comments